Autologous Cultured Epidermis
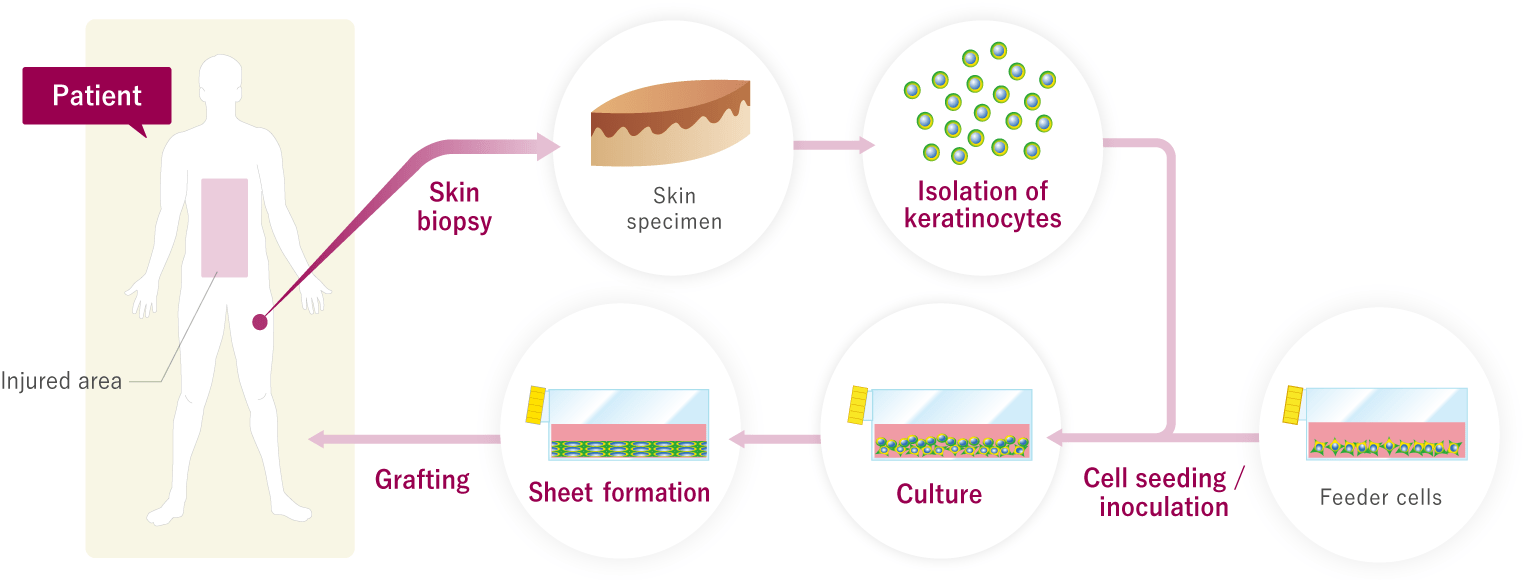
Skin covers the human body completely. An average adult has a total surface area of around 1.6 m2 of skin, which if subcutaneous tissue is included weighs around 9 kg. Skin is the largest organ of the human body. If a burn or other trauma results in skin loss over a wide area, this seriously impairs its vital functions of maintaining body temperature and conserving fluid, and infection by bacteria that invade the body from outside also increases the risk of death. Histologically, skin comprises three layers: from the outside in, these are the epidermis, dermis, and subcutaneous tissue. The keratinocytes that compose the epidermis possess an extremely high ability to proliferate, meaning that skin regenerates very rapidly. When skin is lost over a wide area, however, regeneration takes too long. A cultured epidermis had been developed that can be grafted onto the injured area, made by isolating keratinocytes from a skin biopsy, culturing them in flasks, and forming them into a skin-like sheet.
When cultured epidermis grown from the patient's own cells is grafted, it does not provoke immune rejection but becomes the patient's own skin. Cultured epidermis was originally used to save the lives of patients with severe burns, but the outstanding speed with which it can close wounds, as well as its usefulness in skin pigmentation disorders (thanks to its incorporation of melanocytes*) swiftly became apparent. It was soon being actively used in the treatment of scars, vitiligo, nevi(birthmarks), ulcers, skin-graft donor sites, and other disorders.
Melanocytes: Melanin-producing cells that exist in the basal layer of the epidermis.

Cultured Epidermis
Development
In the 1970s Professor Howard Green of Harvard Medical School developed a method that involved culturing keratinocytes together with mouse fibroblasts* to form a kera-tinocyte sheet, a method now known as Green's technique for culturing epidermis. In 1984 it attracted worldwide attention when the lives of two severely burned children were saved by this technique, which was used to generate 5000-7000 cm2 of cultured epithelium for grafting from what little skin remained to them. Many TEMPs are already available worldwide, and cultured epidermis prepared by Green's technique has invariably played a major role in advancing the development of regenerative medicine in different countries.
Mouse fibroblasts: The 3T3-J2 cell line most favorable to keratinocyte cultivation according to the technique established by Professor H.Green. Their clinical safety has been confirmed in over 20 years of clinical use.
The technology for keratinocyte cultivation has been transferred to J-TEC by Professor Minoru Ueda of Nagoya University. J-TEC members have accumulated their expertise under the guidance of Professor H.Green, who developed the technique, and clinical authority Dr. Michele De Luca, and possesses the skills to generate cultured epidermis using Green's technique to meet the highest global standards.
Culture
By isolating keratinocytes from a 1-cm2 skin sample and culturing them as illustrated below, a sheet of cultured epidermis measuring around 1000 cm2 can be produced in around two weeks.
Transplantation of autologous cultured epidermis
The use and commercialization of the medicinal products developed by Japan Tissue Engineering Co., Ltd. that are referred to on this website are approved only in Japan. A potential use and commercialization in other regions will be subject to the prior granting of a marketing authorization in the given territory and compliance with applicable laws.
Researchers
- Howard Green, M.D.
-
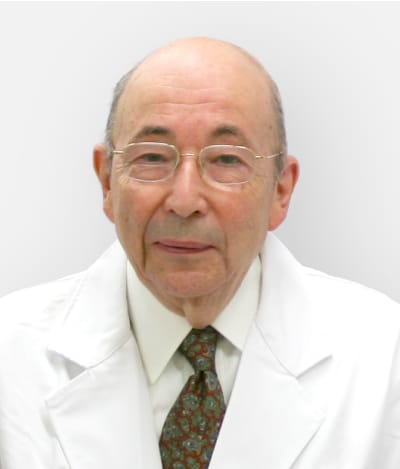
A world authority in the field of epithelial stem-cell biology, and the father of a method now known as Green's technique for culturing epidermis. The late Prof. Green developed a technique that involved culturing keratinocytes together with mouse fibroblasts to form a keratinocyte sheet in the 1970s.
He was Emeritus George Higginson Professor of Cell Biology, Harvard Medical School, U.S.A.
(Dr. Howard Green passed away on October 31, 2015.)
It was in the 1970s when I developed a technique for culturing epidermis, and in 1984, it attracted worldwide attention when the lives of two severely burned children were successfully saved by this technique, which was used to generate 5000-7000 cm2 of cultured epidermis for grafting from what little skin remained to them. More than 20 years have passed since then, and this technique is now starting to play a major role in advancing the development of regenerative medicine in Japan.
I long ago recognized the potential of the company and my impressions were confirmed by my visit to the J-TEC facility. I believe that the company should become a powerful force in the field of cell therapy/regenerative medicine and related fields, not only in Japan, but throughout the world. - Norio Kumagai,
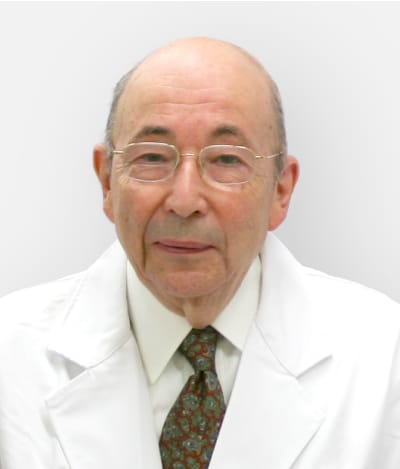
M.D., Ph.D. -

A world authority on the use of cultured epidermis in the clinical treatment.
He is a professor emeritus at St. Marianna University, School of Medicine, JAPAN

Since 1980s, I have been studying the cultivation of epidermal tissue, which was developed in the laboratory by Prof. Howard Green at Harvard University in the United States. In 1985, I reported on the first use of the Green model of cultured epidermis in Japan, which was used in the treatment of severe burn injury. For the last quarter century, autologous and allogeneic cultured epidermis has been used in actual clinical practice for the treatment of nearly 600 cases, including burn injury, scarring, vitiligo, and birthmarks.
Special characteristics of autologous cultured epidermis are the ability to culture from a small epidermal structure to a large volume, and the ability to culture tissue from the patient's own cells, significantly reducing the risk of tissue rejection when it is transplanted to the person who originally provided the starting cells. On the other hand, when culturing the cells of the actual patient, there are individual differences in the ability of the patient's cells to proliferate and grow into viable tissue. We have found an excellent means to make up for these individual differences by using 3T3-J2 cells, which are a Green model of cultured epidermis.
In Japan, there are a very limited number of doctors who have actual experience using tissue engineered medical products. It is my hope that J-TEC will contribute to the creation of systems which will further spread the use of tissue engineered medical products. This can be done through active promotion of activities to enlighten others about this field, including providing information and training to doctors and medical institutions about cell extraction, the art of cell transplantation and the after-care of patients following a transplant, so that doctors can provide the best possible treatment for their patients. - Michele De Luca, M.D.
-

A world authority in the field of stratified epithelial stem-cell biology, Prof.De Luca was the first person in Europe to carry out the transplantation of cultured epithelial stem cells.
He is Professor of Biochemistry, Director of Center for Regenerative Medicine in the Department of Life Sciences, University of Modena and Reggio Emilia, Italy.

I have been providing advices on overall quality control for J-TEC's autologous cultured epidermis and autologous cultured corneal epithelium.
New developments in the technology for managing stem cells mean regenerative medicine is a field with a highly promising future, destined to grow into a major branch of medicine. It will doubtless be an important substitute for organ transplants, although it will never entirely replace them.
Biotechnology companies such as J-TEC that are involved in both regenerative medicine and tissue engineering hold immense potential for growth. My research in collaboration with J-TEC on cultured epidermis that conserves stem cells and melanocytes has convinced me that the company's experienced and highly capable staff will be able to commercialize regenerative medicine successfully. J-TEC has an important role to play in regenerative medicine, both now and in future.

